Ever sat on the toilet and felt a tear-your-heart-out pain that made you afraid to go again? You’re not alone. Anal fissures affect 1 in 10 people seeking help for rectal pain, yet most suffer in silence, thinking their discomfort is “just hemorrhoids.”
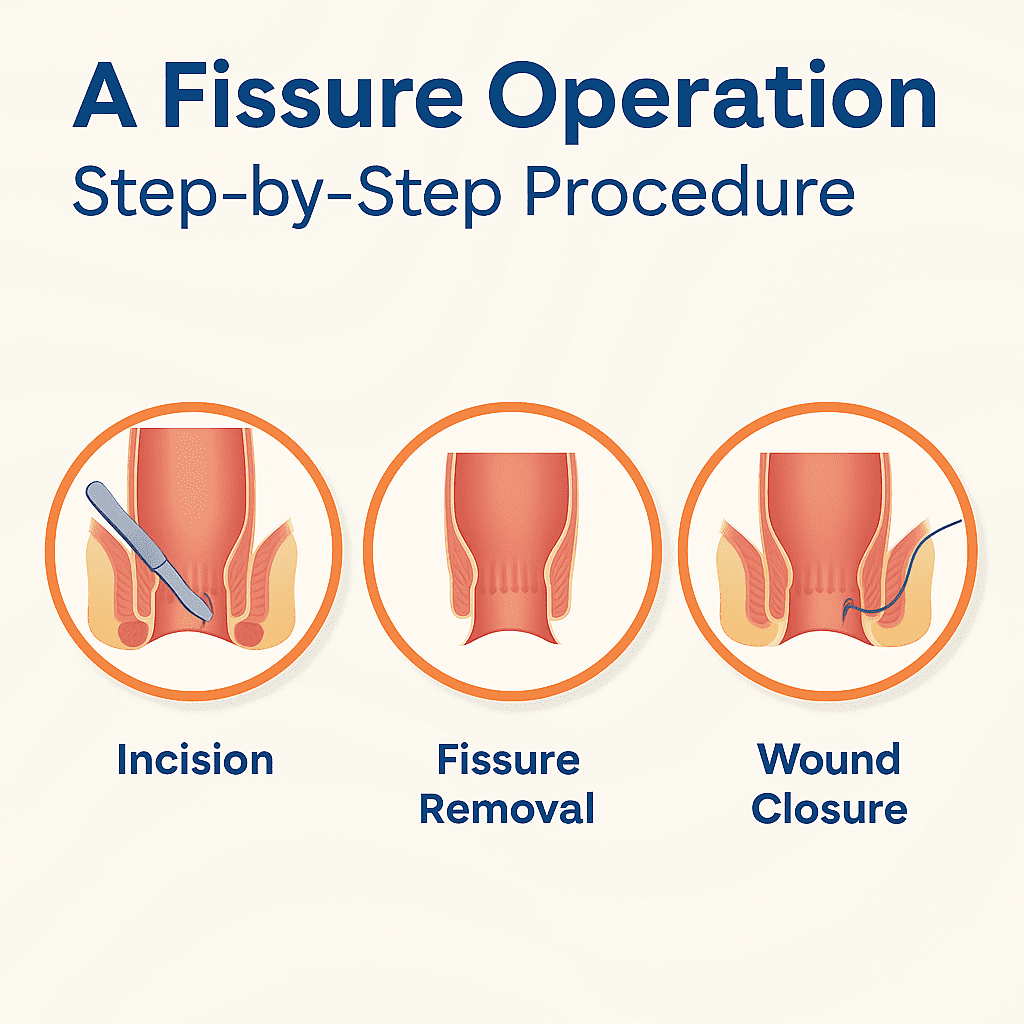
This guide will walk you through everything you need to know about anal fissure operation options – from conservative approaches to surgical interventions when things get serious.
Anal fissures might sound embarrassing, but they’re just small tears in the lining of your anus. Like paper cuts in the worst possible location.
But here’s what your doctor probably isn’t telling you about why these tiny tears sometimes refuse to heal on their own…
Understanding Anal Fissures: What You Need to Know
Definition and Common Causes of Anal Fissures
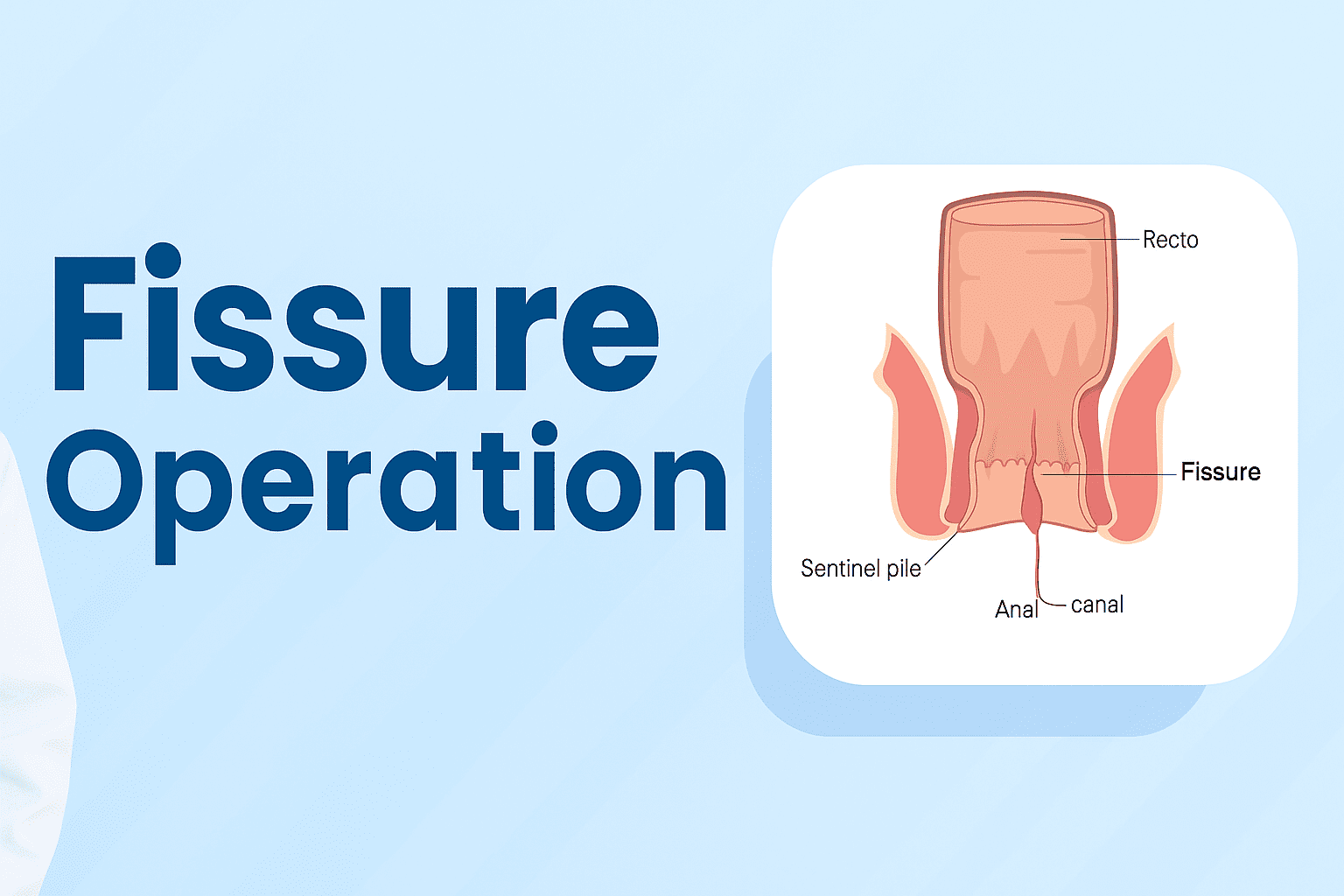
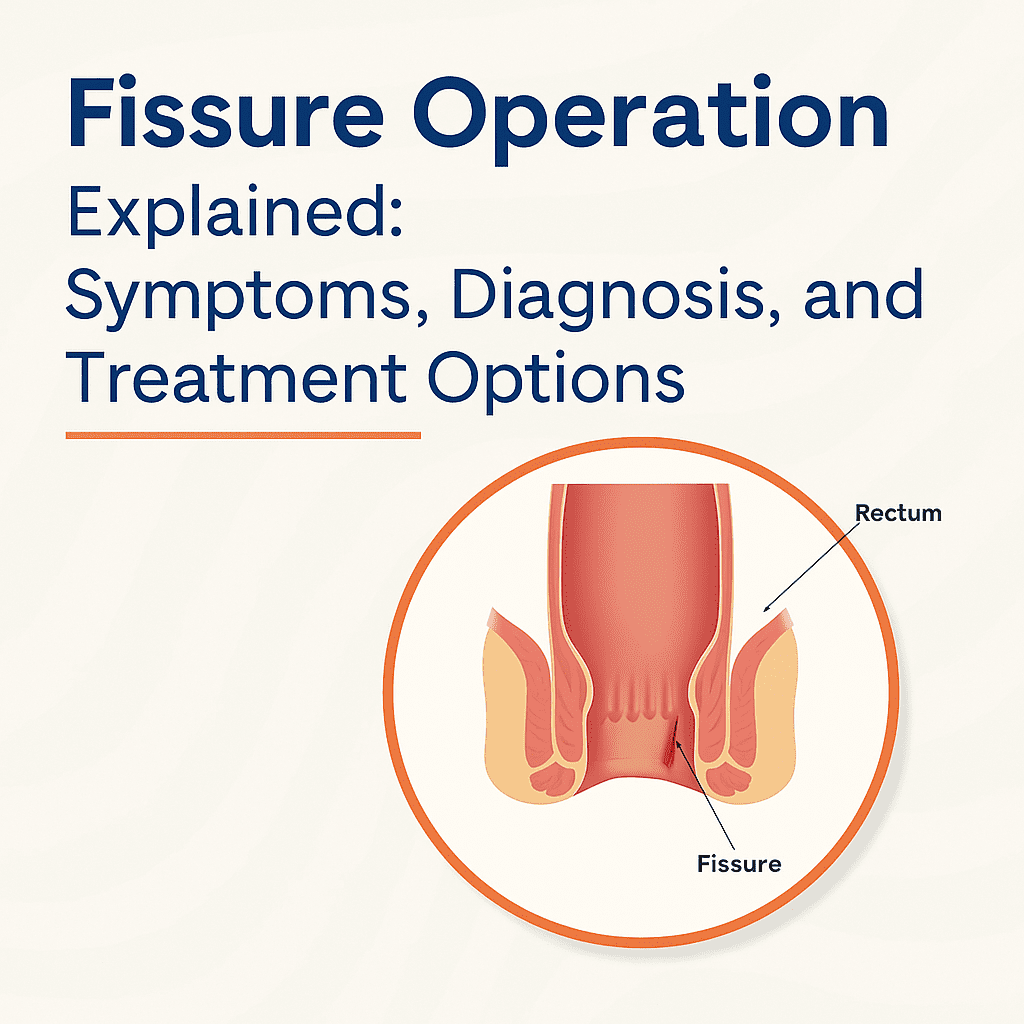
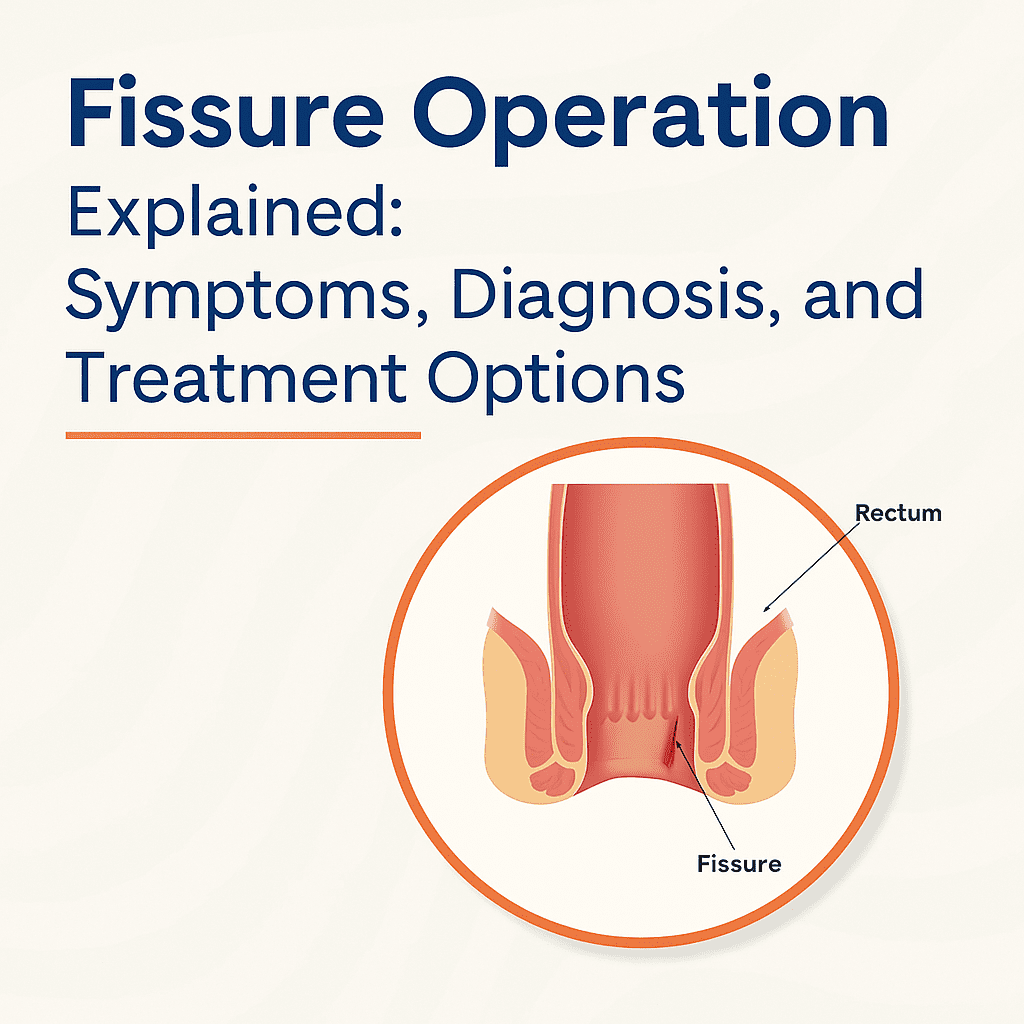
Anal fissures are small tears in the lining of the anus – that thin, delicate tissue at the end of your digestive tract. Think of them like paper cuts, but in a much more uncomfortable location. These tiny tears can cause disproportionate pain, especially during bowel movements when the area stretches.
Most fissures happen for a pretty simple reason: trauma to the anal canal. The number one culprit? Constipation. When you’re straining to pass hard, dry stool, that excess pressure can literally tear the anal lining.
Other common causes include:
- Chronic diarrhea (the frequent irritation damages the tissue)
- Childbirth (especially vaginal deliveries)
- Anal intercourse without proper lubrication
- Inflammatory bowel diseases like Crohn’s disease
- Overly tight anal sphincter muscles
High-Risk Groups and Prevention Strategies
Not everyone faces the same risk when it comes to anal fissures. The truth is, certain groups deal with this painful condition more often:
- Adults between 20-40 years old
- New mothers recovering from childbirth
- People with chronic constipation issues
- Those with inflammatory bowel disease
- Anyone with unusually tight anal sphincter muscles
The good news? Prevention isn’t complicated. Simple lifestyle changes make a huge difference:
- Stay hydrated – Aim for 8 glasses of water daily
- Eat fiber-rich foods – Fresh fruits, vegetables, and whole grains keep things moving
- Exercise regularly – Physical activity promotes healthy bowel function
- Don’t ignore the urge – Holding it in leads to harder stool
- Clean gently – Harsh wiping or soaps can irritate the area
How Fissures Differ from Other Anal Conditions
Anal pain doesn’t always mean you have a fissure. Several conditions affect this area, and telling them apart matters for proper treatment:
| Condition | Key Differences | Pain Pattern |
| Hemorrhoids | Swollen blood vessels, often visible | Dull ache, worse when sitting |
| Anal abscess | Infection causing pus collection | Throbbing, constant pain |
| Anal fistula | Abnormal tunnel between anal canal and skin | Drainage, intermittent pain |
| Anal fissure | Tear in anal lining | Sharp pain during bowel movements |
The distinctive feature of fissures is that knife-like pain during bowel movements, often followed by a burning sensation that can last hours. Many people also notice small amounts of bright red blood on toilet paper.
Impact of Fissures on Quality of Life
The pain from anal fissures goes way beyond physical discomfort. This condition seriously impacts daily life in ways many don’t anticipate:
Many sufferers develop a fear of bowel movements, which only makes constipation worse. This creates a vicious cycle where avoiding the bathroom leads to harder stool, which causes more tearing.
The constant pain affects concentration at work and disrupts sleep patterns. Simple activities like sitting at a desk, exercising, or even walking can become painful challenges.
The intimate nature of the condition often prevents people from seeking help. They suffer silently for months or even years, too embarrassed to discuss their symptoms with healthcare providers.
Relationships suffer too. Intimacy may become painful or impossible, leading to emotional distance between partners. The psychological impact shouldn’t be underestimated – anxiety and depression commonly accompany chronic anal pain.
Recognizing Fissure Symptoms
Primary Warning Signs to Never Ignore
Fissures don’t exactly announce themselves with a megaphone, but they do send clear signals you shouldn’t brush off. The most telling sign? Pain during or after bowel movements that’s often described as “feeling like passing broken glass” or “being cut with a knife.” This isn’t your run-of-the-mill discomfort – it’s sharp, intense, and unmistakable.
Many patients also report seeing bright red blood on toilet paper or in the bowl. Coupled with pain, this blood is a red flag (literally) that something’s wrong.
Another warning sign is muscle spasm in the anal sphincter. These spasms can last for hours after a bowel movement and create a throbbing, aching sensation that makes sitting downright miserable.
Pain Patterns and Characteristics
The pain from an anal fissure follows a pretty distinctive pattern. It typically:
- Starts during bowel movements
- Peaks immediately after
- Gradually fades but may linger for hours
- Returns in a vicious cycle with your next trip to the bathroom
What makes fissure pain unique is its burning, tearing quality. Unlike hemorrhoid discomfort (which tends to be more of a dull ache or pressure), fissure pain has a sharp, cutting edge to it.
Many patients report the pain is so severe they avoid having bowel movements altogether – which only makes things worse by causing constipation and harder stools that further traumatize the area.
Bleeding: When to Be Concerned
Not all bleeding means the same thing. With fissures, blood typically appears as bright red streaks on toilet paper or coating the stool surface. This happens because the tear in the anal lining exposes tiny blood vessels that bleed when irritated during bowel movements.
Here’s when bleeding should raise serious concerns:
- When it’s dark or maroon colored
- If it’s mixed throughout the stool (not just on the surface)
- When bleeding continues well after bowel movements
- If it’s accompanied by dizziness or weakness
Small amounts of bright red blood specifically during bowel movements are typical of fissures, but anything beyond that warrants immediate medical attention.
Chronic vs. Acute Symptom Differences
The difference between acute and chronic fissures isn’t just about time – it’s about how your symptoms evolve.
| Acute Fissures | Chronic Fissures |
| Pain lasts days to weeks | Pain persists beyond 8-12 weeks |
| Bleeding is minimal | Bleeding may increase over time |
| Tissue appears pink/red | Visible scar tissue or skin tag may form |
| Responds well to conservative treatment | Often resistant to basic treatments |
| Minimal sphincter spasm | Persistent, painful sphincter spasms |
Chronic fissures often create a visible “sentinel pile” – a small skin tag at the outer edge of the fissure that’s a dead giveaway to your doctor about what’s happening.
Secondary Symptoms That May Accompany Fissures
While pain and bleeding take center stage, fissures bring along an unwelcome entourage of other symptoms:
- Intense itching around the anal area
- Burning sensation that worsens with movement
- Discharge that may stain underwear
- Difficulty urinating due to pelvic floor muscle tension
- Constipation from fear of painful bowel movements
Many patients also report psychological effects like anxiety about using the bathroom, irritability from chronic pain, and even depression if symptoms persist without relief.
The stress of dealing with these symptoms creates a harmful cycle – anxiety leads to muscle tension, which increases pain, which heightens anxiety further. Breaking this cycle is a crucial part of recovery.
Conclusion:
Anal fissures may start as a small discomfort but can quickly turn into a painful and recurring issue if left untreated. Understanding the symptoms early, getting a proper diagnosis, and exploring the right treatment options—including surgical procedures—can lead to lasting relief. For chronic or non-healing fissures, a fissure operation, especially laser-based treatments, offers a safe and effective solution with faster recovery and minimal discomfort. Always consult a qualified colorectal surgeon to determine the best course of action for your condition. Remember, timely medical intervention can help you return to a pain-free life sooner than you think.