1. Introduction
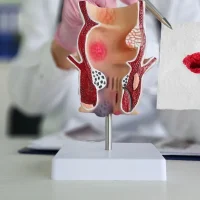
Hemorrhoids, often colloquially referred to as piles, are a common and often debilitating condition affecting millions worldwide. Characterized by swollen and inflamed veins in the rectum and anus, hemorrhoids can cause discomfort, pain, itching, and bleeding. While many mild cases can be managed with lifestyle modifications and conservative treatments, chronic or severe hemorrhoids, particularly those that are prolapsed (protrude outside the anus), frequently require surgical intervention.
For Free Consultation : +91 7670968977
For decades, traditional hemorrhoidectomy, involving the surgical excision of hemorrhoidal tissue, has been the gold standard. While effective, this conventional approach can be associated with significant post-operative pain and a prolonged recovery period. However, advancements in surgical techniques have introduced less invasive alternatives. Among these, stapled hemorrhoidectomy, also known as stapled hemorrhoidopexy or the PPH procedure (Procedure for Prolapse and Hemorrhoids), has emerged as a significant innovation, offering a different paradigm for addressing internal hemorrhoids and prolapsed hemorrhoids. This article will delve into the intricacies of stapled hemorrhoidectomy, exploring its mechanism, benefits, potential risks, and what patients can expect during the recovery process. Our aim is to provide comprehensive, expert-backed information to help individuals and healthcare professionals make informed decisions regarding this modern surgical procedure.
2. What is Stapled Hemorrhoidectomy?
Stapled hemorrhoidectomy, or stapled hemorrhoidopexy, is a surgical procedure designed to treat internal hemorrhoids, particularly those that have prolapsed. Unlike a traditional hemorrhoidectomy, which involves excising the hemorrhoidal tissue itself from the anal margin, stapled hemorrhoidectomy focuses on lifting and repositioning the prolapsed hemorrhoidal cushions back into their anatomical position within the anal canal. The name “hemorrhoidopexy” (pexy meaning fixation) accurately reflects this lifting and fixing action.
The procedure primarily targets internal hemorrhoids, which originate above the dentate line (the line in the anal canal that separates sensitive skin from less sensitive rectal lining). When these internal hemorrhoids become enlarged or prolapse, they can cause symptoms such as bleeding, discomfort, and protrusion.
Comparison with Traditional Hemorrhoidectomy:
The fundamental difference between stapled hemorrhoidectomy and traditional hemorrhoidectomy lies in their approach:
- Traditional Hemorrhoidectomy (Excisional Hemorrhoidectomy): This involves surgically cutting away the swollen hemorrhoidal tissue. It can be performed using various techniques (e.g., LigaSure, Harmonic Scalpel, or conventional scalpel with stitches). While highly effective in removing the hemorrhoids, the open wounds created at the highly sensitive anal margin often lead to significant post-operative pain and a longer healing time. This method is effective for both internal and external hemorrhoids.
- Stapled Hemorrhoidectomy (Stapled Hemorrhoidopexy/PPH): This technique does not remove the hemorrhoids directly. Instead, it involves removing a ring of prolapsed rectal tissue just above the hemorrhoids. By removing this tissue, the hemorrhoids are pulled back up into the anal canal, reducing their prolapse. The staples also disrupt the blood supply to the hemorrhoidal cushions, causing them to shrink over time. Crucially, the excision and stapling occur in an area of the anal canal that has fewer pain-sensitive nerve endings, contributing to less post-operative pain. This procedure is primarily indicated for internal and prolapsed hemorrhoids.
This conceptual difference is key to understanding why stapled hemorrhoidectomy often leads to a more comfortable and quicker recovery for suitable candidates.
3. How Does Stapled Hemorrhoidectomy Work?
The stapled hemorrhoidectomy (or PPH procedure) is an elegant surgical technique that leverages a specialized circular stapling device to address prolapsed internal hemorrhoids. The core principle of the procedure is not to excise the hemorrhoids themselves, but rather to re-suspend the prolapsed hemorrhoidal cushions back into their normal anatomical position and reduce their blood supply.
Here’s a detailed breakdown of the surgical process:
- Anesthesia: The procedure is typically performed under general anesthesia or regional anesthesia (spinal or epidural), ensuring the patient’s comfort and eliminating pain during the surgical procedure.
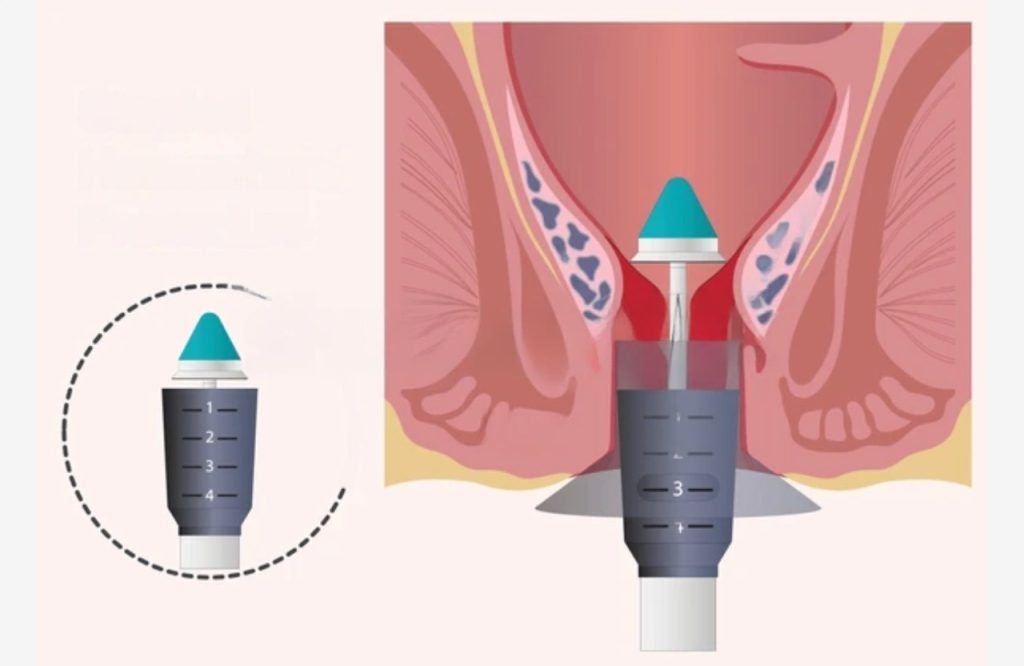
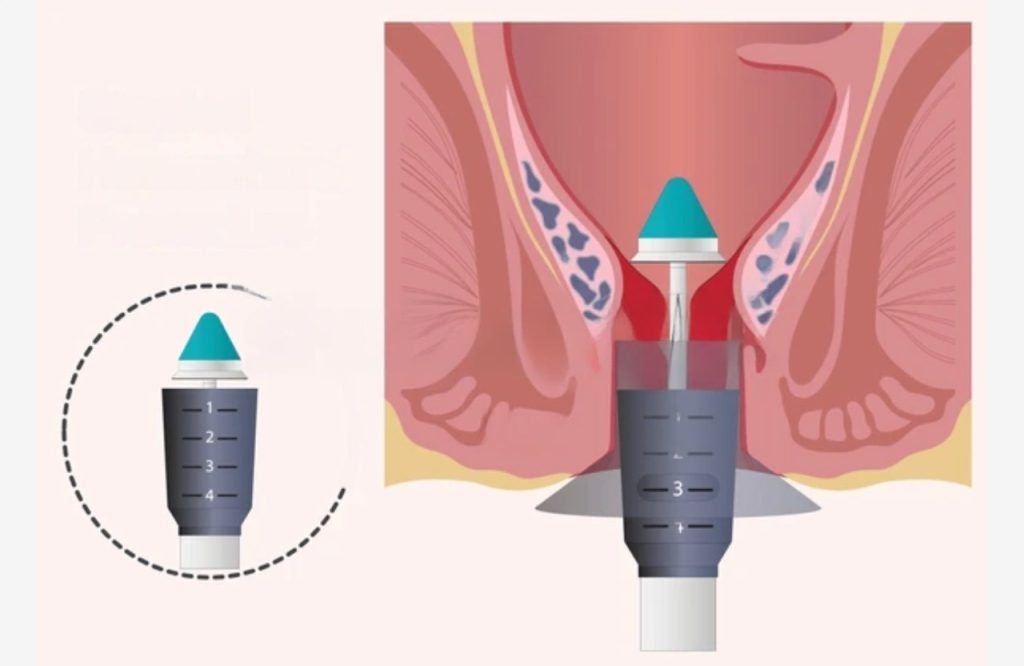
- Anal Dilatation: A circular anal dilator is carefully inserted into the anus. This dilator gently expands the anal canal, providing the surgeon with a clear view and working space.
- Purse-String Suture Placement: Through the dilator, a specialized suture, known as a purse-string suture, is placed circumferentially in the rectal wall, approximately 3-4 cm above the dentate line. This area is chosen because it is relatively insensitive to pain, as it lies above the anal nerve endings. The purse-string suture encompasses the redundant prolapsed rectal mucosa and the underlying hemorrhoidal tissue.
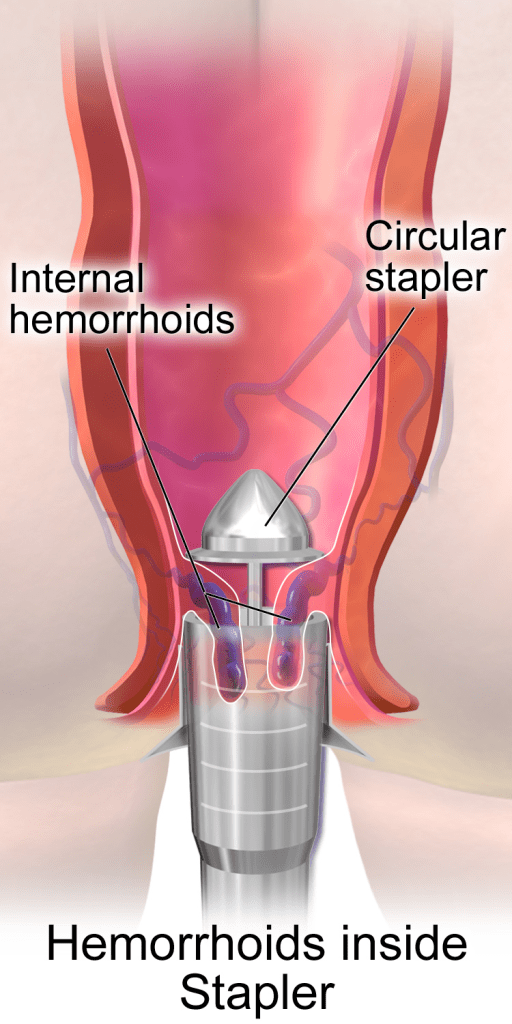
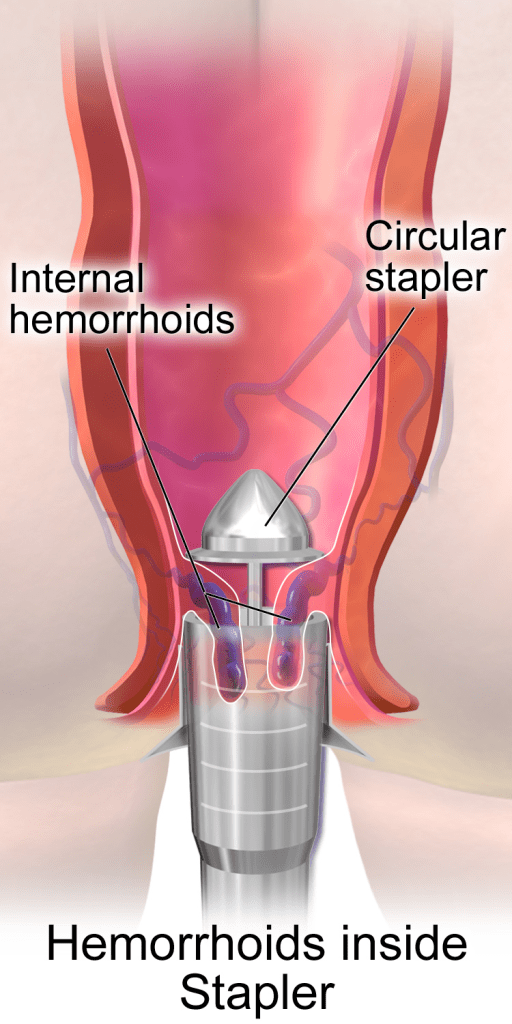
- Stapler Insertion and Excision: The circular stapling device (hemorrhoidal circular stapler) is then introduced into the anal canal, guided by the purse-string suture. The ends of the purse-string suture are threaded through the stapler and tied tightly. This action draws the prolapsed rectal tissue into the housing of the stapler.
- Firing the Stapler: Once properly positioned and the tissue is secured within the stapler, the surgeon fires the device. The stapler simultaneously:
- Excises a ring of the prolapsed rectal mucosa and the underlying redundant submucosal tissue, which includes the upper portion of the enlarged hemorrhoidal cushions.
- Staples (sutures) the cut edges together with two rows of tiny titanium staples, effectively creating a new, elevated anal lining and lifting the hemorrhoids back into place. The staples act as both a cutting and suturing mechanism.
6.Inspection: After the stapler is removed, the surgeon carefully inspects the staple line to ensure hemostasis (control of bleeding) and proper tissue apposition. Any small bleeding points can be controlled with additional sutures.
The removal of the ring of tissue achieves two critical outcomes:
- Lifting and Repositioning: By excising a segment of the rectal mucosa, the prolapsed hemorrhoidal cushions are pulled upwards and fixed in their normal anatomical position within the anal canal. This effectively treats the prolapse.
- Reduced Blood Flow: The stapling action also interrupts some of the arterial blood supply to the hemorrhoidal tissue, causing the hemorrhoids to gradually shrink over time due to reduced engorgement. This is why the procedure is sometimes referred to as hemorrhoidopexy, emphasizing the repositioning rather than complete excision.
This precise and controlled mechanism makes the PPH procedure a highly effective and often preferred alternative to traditional hemorrhoidectomy for appropriate cases of internal hemorrhoids and prolapsed hemorrhoids.
4. Benefits of Stapled Hemorrhoidectomy
Stapled hemorrhoidectomy, also known as stapled hemorrhoidopexy or the PPH procedure, offers several significant advantages over traditional excisional hemorrhoidectomy, making it a compelling option for many patients suffering from internal hemorrhoids and prolapsed hemorrhoids. These benefits primarily stem from its unique surgical approach, which avoids open wounds at the highly sensitive anal margin.
Here are the key advantages:
- Significantly Less Post-operative Pain: This is arguably the most cited and appreciated benefit of stapled hemorrhoidectomy. Because the surgical incision and stapling occur above the dentate line, in an area with fewer pain-sensitive nerve endings, patients typically experience considerably less pain compared to traditional hemorrhoidectomy. This often translates to reduced reliance on strong pain medication and a more comfortable recovery.
- Faster Recovery and Return to Normal Activities: The absence of open wounds at the anal verge allows for a much quicker healing process. Patients undergoing stapled hemorrhoidectomy often report a faster return to work and daily activities. While traditional hemorrhoidectomy can necessitate several weeks off work, many patients undergoing stapled hemorrhoidectomy are back to light activities within a few days to a week. The overall recovery period is significantly shortened.
- Reduced Bleeding: The stapler simultaneously cuts and seals the tissue, which minimizes intraoperative and immediate post-operative bleeding. This contributes to a cleaner surgical field and reduced complications related to blood loss.
- Shorter Hospital Stay: Due to less pain and faster initial recovery, many stapled hemorrhoidectomy procedures can be performed on an outpatient basis or with just an overnight stay, contrasting with the longer hospitalizations sometimes required for traditional surgery.
- Improved Anal Function and Cosmesis: By repositioning the hemorrhoidal tissue and not excising external skin, the procedure helps preserve the normal anatomy of the anal canal. This can lead to better anal function post-surgery and a more aesthetically pleasing outcome compared to traditional methods that might involve removal of perianal skin.
- Effective for Prolapsed Hemorrhoids: The PPH procedure is particularly effective for prolapsed hemorrhoids, as it directly addresses the underlying issue of mucosal prolapse by lifting and securing the tissue back in place.
- Fewer Post-operative Dressings and Wound Care: Without open wounds, the need for frequent dressing changes and complex wound care is significantly reduced, simplifying the post-operative regimen for patients.
These combined benefits underscore why stapled hemorrhoidectomy has become a preferred surgical procedure for many individuals dealing with the discomfort and complications of advanced internal hemorrhoids and prolapsed hemorrhoids. It represents a significant step forward in making hemorrhoid surgery a less daunting experience.
5. Who is a Good Candidate for Stapled Hemorrhoidectomy?
While stapled hemorrhoidectomy offers numerous advantages, it is not universally applicable to all types or grades of hemorrhoids. Patient selection is crucial for maximizing the benefits and minimizing complications. A thorough evaluation by a qualified colorectal surgeon is essential to determine if the PPH procedure is the most appropriate surgical procedure for an individual.
Generally, a good candidate for stapled hemorrhoidectomy typically presents with:
- Internal Hemorrhoids, especially Grade II, III, or IV:
- Grade II Hemorrhoids: These prolapse during defecation but spontaneously reduce.
- Grade III Hemorrhoids: These prolapse during defecation and require manual reduction.
- Grade IV Hemorrhoids: These are permanently prolapsed and cannot be manually reduced. Stapled hemorrhoidectomy is particularly effective for these grades where the primary problem is prolapse of the internal hemorrhoidal cushions.
- Significant Prolapse of Hemorrhoidal Tissue: The procedure is designed to treat the underlying prolapse of rectal mucosa and associated hemorrhoids. Patients whose main symptom is prolapse, rather than just bleeding or external swelling, are often excellent candidates.
- Failure of Conservative Treatments: Patients who have tried and failed to achieve satisfactory relief from non-surgical interventions (such as dietary changes, fiber supplements, topical creams, rubber band ligation, or sclerotherapy) are often considered for surgical options.
- Absence of Large External Hemorrhoids or Skin Tags: Stapled hemorrhoidectomy primarily targets internal hemorrhoids and the prolapsed rectal mucosa. It is generally not indicated for isolated large external hemorrhoids or prominent skin tags, as these would require separate excision if they are symptomatic. In some cases, a combined approach might be considered.
- Good General Health: As with any hemorrhoid surgery, candidates should be in good overall health, free from significant co-morbidities that would increase surgical risk. Conditions that might impair healing or increase bleeding risk (e.g., severe coagulopathy, active inflammatory bowel disease in the perianal area) may be contraindications.
- No Active Perianal Infections: Any active infections in the anal or perianal area should be treated and resolved before considering this elective surgical procedure.
- Realistic Expectations: Patients should have a clear understanding of the procedure, its potential benefits, and the realistic recovery timeline.
It’s important to note that a detailed physical examination, including an anoscopy or proctoscopy, is vital for proper assessment. The surgeon will evaluate the size, grade, and extent of the internal hemorrhoids and prolapsed hemorrhoids to determine the suitability for stapled hemorrhoidopexy (PPH procedure). While its advantages are compelling, a personalized assessment ensures the best possible outcome for the individual patient.
6. Risks and Complications of Stapled Hemorrhoidectomy
While stapled hemorrhoidectomy (PPH procedure) is widely considered a safe and effective surgical procedure for internal hemorrhoids and prolapsed hemorrhoids, like any surgery, it carries potential risks and complications. It’s crucial for patients to be fully informed of these possibilities before making a decision about hemorrhoid surgery.
Common Risks and Complications (generally less severe):
- Pain: Although significantly less than traditional hemorrhoidectomy, some pain and discomfort in the anal region are expected post-surgery. This is usually manageable with oral pain medication.
- Bleeding: Minor bleeding, especially during bowel movements, is common for the first few days to a week. Rarely, more significant bleeding may occur, potentially requiring intervention.
- Urinary Retention: Difficulty urinating after surgery can occur, often due to anesthesia effects or local discomfort. This is usually temporary.
- Thrombosed External Hemorrhoids/Skin Tags: While the procedure targets internal hemorrhoids, new external hemorrhoids or skin tags can sometimes form, or existing ones can become symptomatic, especially if there’s significant edema.
- Fecal Urgency or Frequent Bowel Movements: Some patients might experience temporary changes in bowel habits, including a feeling of urgency or needing to go more frequently.
- Anal Spasm: Involuntary contraction of the anal sphincter muscles can cause discomfort.
Less Common but More Serious Complications:
- Staple Line Bleeding: Though rare, significant bleeding from the staple line can occur, sometimes requiring further intervention to control.
- Staple Line Stricture: Narrowing of the anal canal at the staple line, leading to difficulty with bowel movements. This may require dilatation or further surgery.
- Perforation of the Rectum: A very rare but serious complication where the stapler accidentally creates a hole in the rectal wall, potentially leading to peritonitis (infection of the abdominal cavity). This is a surgical emergency.
- Fistula Formation: The development of an abnormal tunnel between the rectum and the skin (rectovaginal or rectourethral fistula) is an extremely rare but severe complication.
- Infection: Although prophylactic antibiotics are often given, infection at the surgical site is a rare but possible risk.
- Recurrence of Prolapse or Hemorrhoids: While the procedure is effective, there’s always a possibility that the prolapse or hemorrhoids may recur over time, especially if underlying causes are not addressed. Studies suggest recurrence rates comparable to or slightly higher than traditional hemorrhoidectomy in the very long term, but with significantly better short-term recovery.
- Persistent Pain: Chronic pain after stapled hemorrhoidectomy, though rare, can occur and may require further investigation and management.
Comparison with Traditional Hemorrhoidectomy Complications:
When comparing complications, stapled hemorrhoidectomy generally has:
- Lower incidence of severe post-operative pain.
- Lower incidence of prolonged wound healing issues (since there are no open wounds at the anal margin).
- Potentially a slightly higher, though still low, risk of specific complications like staple line stricture or rectal perforation (due to the device use), though this is largely mitigated by surgeon experience and proper technique.
- Similar or slightly higher rates of recurrence in the very long term, but with a significantly better short-term recovery.
Choosing an experienced surgeon with a proven track record in performing stapled hemorrhoidopexy (PPH procedure) is paramount in minimizing these risks and complications. Open communication with your healthcare provider about all potential outcomes is essential for informed decision-making regarding this surgical procedure.
7. Recovery Process after Stapled Hemorrhoidectomy
The recovery process following stapled hemorrhoidectomy is typically characterized by less pain and a quicker return to normal activities compared to traditional hemorrhoid surgery. However, it’s crucial for patients to understand what to expect and diligently follow post-operative care instructions to ensure optimal healing and minimize complications.
Immediate Post-Operative Period (First 24-48 hours):
- Pain Management: While pain is significantly less than traditional methods, some discomfort and pressure in the rectum are common. This can usually be managed effectively with prescribed oral pain medication (e.g., NSAIDs, mild opioids).
- Discharge: Many patients can be discharged on the same day as the surgical procedure or after an overnight stay, depending on their recovery and surgeon’s preference.
- Diet: A light, high-fiber diet is generally recommended to promote soft bowel movements. Adequate hydration is also crucial.
- Bowel Movements: The first bowel movement may be uncomfortable. Stool softeners and laxatives are typically prescribed to ensure soft stools and prevent straining, which could disrupt the staple line.
- Slight Bleeding/Discharge: It’s normal to experience a small amount of bright red bleeding, especially with bowel movements, and some serosanguinous (pinkish) discharge for the first few days. A pad may be worn for comfort.
First Week of Recovery:
- Activity: Most patients can return to light daily activities within 2-3 days. Strenuous activities, heavy lifting, and prolonged sitting should be avoided for at least a week to prevent straining and pressure on the surgical site.
- Hygiene: Gentle cleansing of the anal area after each bowel movement with soft toilet paper or a bidet is recommended. Warm sitz baths (soaking in a shallow tub of warm water) for 15-20 minutes, 2-3 times a day, can help relieve discomfort and promote healing.
- Staple Passage: The small titanium staples used in the PPH procedure will typically pass naturally in the stool over the next 1-2 weeks as the tissue heals. Patients usually won’t notice them.
Weeks 2-4 and Beyond:
- Return to Work: Depending on the nature of their job, many patients can return to work within 3-7 days, especially for sedentary roles. Physically demanding jobs may require a longer absence.
- Full Activities: Most patients can resume normal physical activities, including exercise, within 2-4 weeks, as advised by their surgeon.
- Follow-up Appointments: A follow-up visit with the surgeon is usually scheduled within 1-2 weeks post-surgery to check the healing progress and address any concerns. Further follow-ups may be scheduled as needed.
- Long-term Care: Maintaining a high-fiber diet, adequate hydration, and avoiding straining during bowel movements are crucial long-term measures to prevent recurrence of internal hemorrhoids or prolapsed hemorrhoids.
Potential Issues During Recovery:
- Persistent Pain: While less common, if pain is severe or persistent, contact your surgeon.
- Excessive Bleeding: Any heavy bleeding, clots, or bleeding that doesn’t stop should be reported to your surgeon immediately.
- Difficulty with Bowel Movements: If stool softeners and laxatives are not effective, or if you experience significant straining, seek medical advice.
- Signs of Infection: Fever, increased pain, redness, or pus around the anus should prompt immediate medical attention.
By adhering to the post-operative care guidelines, patients can generally expect a smooth and relatively comfortable recovery after stapled hemorrhoidectomy, enabling a quicker return to their normal lifestyle and significant relief from the symptoms of their hemorrhoidal tissue issues.
8. Conclusion
Stapled hemorrhoidectomy, or stapled hemorrhoidopexy (PPH procedure), represents a significant advance in the surgical procedure landscape for chronic and symptomatic internal hemorrhoids, particularly those characterized by prolapsed hemorrhoids. By strategically repositioning the redundant rectal mucosa and reducing blood supply rather than excising the hemorrhoidal tissue directly at the sensitive anal margin, this technique offers a compelling alternative to traditional hemorrhoid surgery.
The primary advantages are clear: significantly less post-operative pain, a notably faster recovery period, and a quicker return to daily activities. These benefits contribute to a more comfortable and less disruptive treatment experience for patients. While the procedure is effective for addressing the prolapse and associated symptoms, it’s essential to understand that, like any surgical intervention, it carries potential complications, though many are rare and manageable. Long-term success also hinges on adherence to post-operative care and lifestyle modifications.
For individuals grappling with persistent discomfort, bleeding, or the inconvenience of prolapsed hemorrhoids that have not responded to conservative treatments, stapled hemorrhoidectomy presents a viable and often preferred solution. Its focus on anatomical restoration combined with reduced invasiveness has cemented its role in modern proctological practice.
9. Call to Action
If you are experiencing symptoms of chronic or severe hemorrhoids, particularly if you suspect internal hemorrhoids or prolapsed hemorrhoids, and are considering surgical options, it is crucial to seek expert medical advice.
Consult with a qualified colorectal surgeon today at SurgiKure to discuss whether stapled hemorrhoidectomy (PPH procedure) is the right treatment for your specific condition. An individualized assessment will determine the most appropriate surgical procedure and ensure you receive comprehensive care tailored to your needs.
Don’t let hemorrhoids dictate your comfort and quality of life. Take the first step towards lasting relief.


Naszenaturalne
Absolutely charming.